April 2012
General Principles
The clinical skills evaluation requirement is effective for residents who entered residency training (PGY-2 for neurology, PGY-3 for child neurology) on or after July 1, 2005. The clinical skills evaluation requirement is also effective for residents who entered a combined residency training program (Neurology/Internal Medicine; Neurology/Diagnostic Radiology/Neuroradiology; Neurology/Psychiatry; Neurodevelopmental Disabilities) as a PGY-1on or after July 1, 2004, or as a PGY-2 on or after July 1, 2005, regardless of the rotations they actually have in those years.
The American Board of Psychiatry and Neurology (ABPN) requires that residents demonstrate mastery of these three clinical skills to apply for certification in the specialties of neurology and neurology with special qualification in child neurology:
- Medical interviewing skills
- Neurological examination skills
- Humanistic qualities, professionalism, and counseling skills
Demonstration of competency in evaluating a minimum of five different patients (as specified below) during residency training is required. (Videotaped interactions or simulated/standardized patients cannot be used as the basis for the evaluations.) Training programs may elect to do more such evaluations. They may also assess additional competencies in the evaluation.
Required Clinical Skills Evaluations for Child Neurology
Child Neurology Residents
- Critical care: One critically ill child patient with neurological disease (may be in either an intensive care unit or emergency department setting or an emergency consultation from another inpatient service)
- Neuromuscular: One child patient with a neuromuscular disease (may be in either an inpatient or outpatient setting)
- Ambulatory: One child patient with an episodic disorder, such as seizures or migraine (most likely in an outpatient setting)
- Neurodegenerative: One child patient with a neurodegenerative disorder, such as an inherited degenerative disease (most likely in an outpatient setting)
- Adult patient: One adult patient with a neurological disorder (most likely in an outpatient setting)
At least one of the above child patients must be from each of these age groups:
- An infant or child aged younger than two
- A child aged two to ten
- An adolescent (aged 11 – 18)
The selection of patients (outlined above) by age is at the discretion of the residency program director.
Selection of Patient
The patients must be unknown to the resident. While it is preferable that the patients have not been seen previously by any resident, patients previously seen at the institution may be asked to participate in the evaluation process. Whenever possible, patients with conversion disorders or somatoform disorders should not be selected. The selection of patients is at the discretion of the residency director.
Evaluators
Each of the five evaluations must be conducted by an ABPN-certified neurologist/child neurologist. All evaluators must be currently diplomates of the ABPN. Evaluations involving adult patients may be done by either adult or child neurologists. Evaluations involving child patients must be completed by child neurologists. At least three of the five evaluations must be conducted by different ABPN-certified neurologists/child neurologists. The evaluator must observe the resident’s performance and score the resident’s medical interviewing skills; neurological examination skills; humanistic qualities/professionalism/counseling skills; and presentation/formulation.
Duration of Each Encounter
Each evaluation session should last approximately one hour. The residents should be given up to 45 minutes to conduct the history and neurological examination. Thereafter, he/she should have 10-15 minutes to present a summary of the important findings on history and neurological examination. The remainder of the time should be spent in discussion and feedback from the evaluator who observed the encounter.
While the evaluator may wish to discuss the diagnosis, differential diagnosis, and plans for evaluation and treatment with the resident, these steps are not required by the ABPN. The resident does not need to demonstrate proficiency in these aspects of the encounter to pass the clinical skills evaluation.
Timing of the Evaluations
The evaluations may be administered at any time during residency training; however, the ABPN encourages administering them early in training. The ABPN anticipates that many residents may not perform acceptably on all their evaluations on the first attempt.
Evaluation Forms
Evaluations must be completed on ABPN-approved forms, and two versions (NEX v.1 and NEX v.2) are posted on the ABPN web site. Residency programs can add additional competencies/items for their own purposes. If programs develop their own forms, they must be submitted to the ABPN for approval.
Determination of Acceptable Performance
The individual evaluator will determine if the resident performed acceptably on all three components (medical interviewing, neurological examination, humanistic qualities/ professionalism/counseling skills) of the clinical evaluation.
An acceptable score is required for all three components. Regardless of when during training the resident takes the evaluation, the standard for acceptable performance that of a competent practicing neurologist/child neurologist remains the same.
Because the resident may take each of these clinical skills evaluations multiple times if necessary (which will not affect the resident’s admissibility to the ABPN certification examination), there should not be pressure to score a resident’s performance as acceptable on an evaluation.
If a resident is unsuccessful in completing the evaluations, any remediation activities are the responsibility of the training program.
Submission of Documentation to the ABPN
At the time of application for certification, the ABPN requires attestation from the residency director that the resident performed acceptably on all five clinical skills evaluations.
Documentation must include the category of patient, the date of successful completion, and the full names of the ABPN-certified evaluators. For child neurologists, the age of the patient must also be recorded. It is recommended that the program retain the evaluation forms as part of the resident’s training file. The ABPN reserves the right to audit the evaluation process. The evaluations are valid for seven years following completion of residency training.
Documentation for neurology candidates must be received from the program director of an ACGME-accredited neurology residency program. Documentation for child neurology candidates must be received from the program director of an ACGME-accredited child neurology residency program.
Components of the Clinical Skills Evaluation and Scoring Criteria
A. Medical Interviewing Skills
The ability to obtain a clear history is a fundamental component of the core competency of patient care. The art of being an excellent neurologist is the ability to make an accurate localization of the patient’s neurological illness and to reach a most likely diagnosis based on the patient’s history. The evaluator must observe the resident’s skill and thoroughness in obtaining the history.
The ABPN recognizes that neurologists may use several different strategies to obtain the history from a patient and that the approach may vary among patients. Thus, the ABPN requires that residents successfully demonstrate the ability to perform a thorough and accurate history in a minimum of five encounters.
The resident is expected to ask about the chief complaint, the history of the present illness, past medical history, family history, and social history and conduct a review of systems. The quality and completeness of the information collected from all components of the history should be evaluated. The ABPN expects the resident to skillfully obtain the history. While the history should emphasize the patient’s neurological illness, relevant components of other aspects should be mentioned. For example, if the patient has had a stroke, it is relevant to ask about hypertension, heart disease, family history of stroke, smoking, and recent cardiac complaints.
Depending upon the patient, the resident may use very direct or open-ended questions. The technique used by the resident to obtain the historical information reflects the resident’s ability to communicate with the patient as well as his/her ability to change techniques to obtain the necessary information.
The resident must not review prior medical records in order to obtain the patient’s history. The focus of this evaluation is on the ability of the resident to obtain the history from a “new” patient and/or family members, as would be done in practice.
The resident is expected to obtain information about the duration and course of the neurological illness and the types of neurological symptoms. While a chronological approach often is desirable, different strategies are acceptable. If appropriate, the resident should obtain information about any incident or event that may have precipitated the neurological problems. If it is a long-standing illness, the resident should ask about recent changes. If it is an episodic disorder, information about the number and types of events, provocations, duration of symptoms, etc. should be obtained. The resident should ask questions that probe for both important positive (presence of) and important negative (absence of) symptoms or components of the neurological history. These include pain, loss of consciousness, weakness, etc. Information about prior treatment (medications, surgery, etc.) can provide important diagnostic clues.
- Did the resident miss important historical clues offered by the patient?
- Did the resident follow-up on components of the history?
At the end of the history, both the resident and the evaluator should have a clear understanding of the nature of the patient’s neurological illness.
|
Score |
Scoring Criteria for Medical Interview |
|
8 (Outstanding) |
History performed with no deficiencies or errors and provided a clear understanding of the patient’s neurological illness. |
|
7 (Excellent) |
A few minor deficiencies or errors in the history. |
|
6 (Very good) |
Minor deficiencies or errors in the history. |
|
5 (Acceptable) |
Deficiencies or errors in the history but enough information obtained to formulate the case. |
|
4 (Borderline but unacceptable) |
Deficiencies or errors in the history resulting in missing information. |
|
3 (Unsatisfactory) |
Major deficiencies or errors in the history resulting in missing important information. |
|
2 (Poor) |
Omitted major portions of the history resulting in inadequate understanding of the case. |
|
1 (Very poor) |
History done so poorly that the resident could not understand the case. |
A score of 5 or greater is required to pass this component of the clinical skills evaluation.
B. Neurological Examination Skills
The ability to perform a thorough examination is a major component of the core competency of patient care. For a neurologist, the ability to do a neurological examination is a fundamental clinical skill.
The ABPN recognizes that there are different approaches to the neurological examination and no particular style, sequence, or organization is required. However, the ABPN expects the neurological examination to be thorough and to assess mental status, station and gait, motor, sensory, coordination (cerebellar), cranial nerves, and reflexes. In some circumstances, such as a wheelchair bound patient, parts of the examination may be omitted. While the ABPN expects that all aspects of the examination will be performed, components of the examination should reflect the nature of the patient’s problem (as obtained from the history). For example, the resident may wish to do a more detailed mental status examination in a patient with a chief complaint of memory loss than in a patient with symptoms of a tardy ulnar palsy.
The resident should not be expected to do a general physical examination although in some circumstances, components of the general examination may be relevant to the patient’s presentation. For example, the resident may wish to auscultate for bruits in a patient with a TIA.
The resident’s interactions with the patient during the examination should be assessed.
- Was the resident rough? For example, did the resident examine a painful leg to the obvious discomfort of the patient, despite being warned not to do so?
- Did the resident do components of the examination in the correct manner?
- Did the resident use the appropriate instruments, and were they used correctly?
- Were major relevant portions of the examination missed?
- Did the resident detect the relevant neurological signs?
- Did the resident ignore or misinterpret some of the neurological findings?
- Did the resident adjust the examination in response to previously detected signs?
- Did the findings of the examination prompt the resident to ask additional history?
- Did the findings of the examination prompt reconsideration of the location or nature of the neurological illness?
At the end of the examination, both the resident and the evaluator should have a clear understanding of the location and nature of the patient’s neurological illness. The findings on the examination should be compatible with the patient’s neurological history.
|
Score |
Scoring Criteria for Neurological Examination |
|
8 (Outstanding) |
Neurological examination performed with no detected shortcomings. |
|
7 (Excellent) |
A few minor deficiencies or errors in the neurological examination. |
|
6 (Very good) |
Minor deficiencies or errors in the neurological examination. |
|
5 (Acceptable) |
Deficiencies or errors in the neurological examination but enough information obtained to formulate the case. |
|
4 (Borderline but unacceptable) |
Deficiencies or errors in performing the neurological examination resulting in missing information. |
|
3 (Unsatisfactory) |
Major deficiencies or errors in performing the neurological examination resulting in missing important information. |
|
2 (Poor) |
Omitted major portions of the neurological examination resulting in inadequate understanding of the case. |
|
1 (Very poor) |
Neurological examination was so poorly done that the resident did not understand the case. |
A score of 5 or greater is required to pass this component of the clinical skills evaluation.
C. Humanistic Qualities/Professionalism/Counseling Skills
The ability to communicate effectively with patients and families is one of the six core competencies for physicians. Effective communication is a key component of a physician’s interpersonal skills and in the development of an appropriate patient-doctor relationship.
The communication skills of the resident should be assessed throughout the patient encounter. The communication can include both verbal and non-verbal means. For example, being rough during the examination can convey a lack of skill in communication. The resident’s performance should be scored in light of the patient’s ability to cooperate with the examination. While there is no set criterion for passing this competency, the overall performance should be the basis for grading this clinical skill.
The resident should be sensitive to ethnic, racial, religious, or cultural issues. The resident should also be aware of educational, language, or community issues that may affect the patient’s ability to communicate. The resident should take steps or employ strategies that deal with these issues and at the same time permit an accurate history and examination. If the patient does not speak English, the resident should seek other ways to communicate with the patient, such as the use of a translator or talking to family members who are proficient in English
The dialogue between the patient and the resident should be evaluated.
- Did the resident make the patient and family feel as comfortable as possible in the situation?
- Did the resident interact in a neutral or positive way with the patient?
- Did the resident demonstrate respect for the patient and family?
- Was the resident rude, brusque or demanding?
- Did the resident interrupt the patient during the history?
- Did the resident fail to follow-up on the patient’s comments?
- Did the resident allow the patient to respond to questions?
- Did the resident revise or reformat questions when it appeared that the patient did not understand?
- Did the resident direct questions to family members if it appeared that the patient did not have information about part of the history?
- Did the resident explain the components of the neurological examination and give clear instructions?
|
Score |
Scoring Criteria for Humanistic Qualities/Professionalism/Counseling Skills |
|
8 (Outstanding) |
Effective communication skills and patient-doctor interactions. |
|
7 (Excellent) |
A few minor problems in communication or patient-doctor interactions. |
|
6 (Very good) |
Minor problems in communication or patient-doctor interactions. |
|
5 (Acceptable) |
Had problems in communication or patient-doctor interactions but still established rapport. |
|
4 (Borderline but unacceptable) |
Had problems in communication or patient-doctor interactions, rapport with patient was borderline or not good. |
|
3 (Unsatisfactory) |
Major problems in communication or patient-doctor interactions, unable to establish rapport with patient. |
|
2 (Poor) |
Major problems with communication, rude or unpleasant to patient. |
|
1 (Very poor) |
Interactions or communication with the patient were so bad that the evaluator needed to intervene. |
A score of 5 or greater is required to pass this component of the clinical skills evaluation.
D. Presentation/Formulation
The ABPN does not require that residents perform acceptably on this component, but it has been included on the ratings. The ABPN does not require that residents perform acceptably on this component, but it has been included on the rating forms and guidelines for scoring are provided because residents will have to present the results of the history and physical examination.
|
Score |
Scoring Criteria for Presentation/Formulation |
|
8 (Outstanding) |
No major deficiencies in the description of the key findings of the history and neurological examination. |
|
7 (Excellent) |
One minor deficiency in the description of the key findings of the history or neurological examination. |
|
6 (Very good) |
Two minor deficiencies in the description of the key findings of the history or neurological examination. |
|
5 (Acceptable) |
A few minor deficiencies or one major deficiency in the description of the key findings of the history or neurological examination. |
|
4 (Borderline but unacceptable) |
Several minor deficiencies or two major deficiencies in the description of the key findings of the history or neurological examination; missed some points. |
|
3 (Unsatisfactory) |
Several major deficiencies in the description of the key findings of the history or neurological examination; missed several points. |
|
2 (Poor) |
Multiple major deficiencies in the description of the key findings of the history or neurological examination; summary of findings was incomprehensible. |
|
I (Very poor) |
Numerous major deficiencies in the description of the key findings of the history or neurological examination; summary of findings was incomprehensible. |
A score of 5 or greater is required to pass this component of the clinical skills evaluation.
Post-Residency Clinical Skills Evaluation
Residency directors may administer clinical skills evaluations for graduates of their programs or of other programs. All of the requirements for in-training evaluations will apply. Documentation of successful completion must be received from the respective neurology/child neurology program director. The fifth evaluation must be completed within five years of the first evaluation, and they are valid for seven years after completion of the fifth clinical skills evaluation.
Resident Wellbeing
- What is resident wellbeing?
- How do we maintain it?
- What worked or you in the past?
- What are your stressors?
- What are your supports
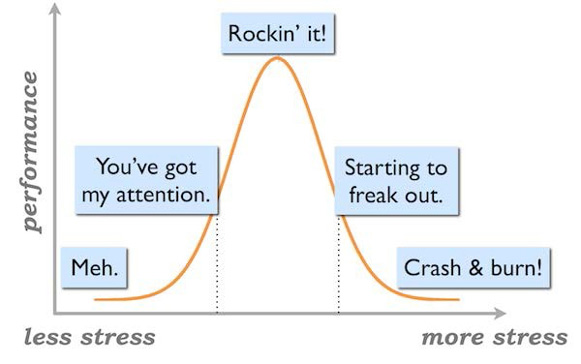
Striking a Balance
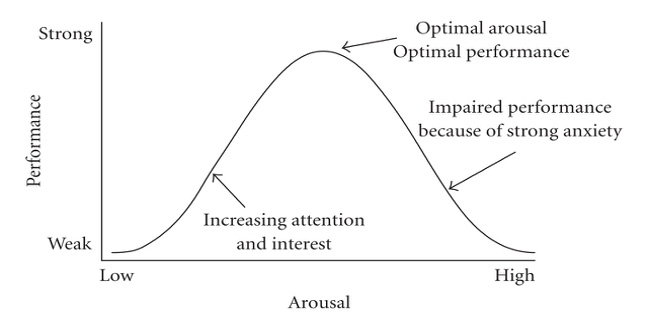
Finding the Sweet Spot
General Resources
- NYP BeHealthy Wellness Initiative (on infonet)
- Yoga/Relaxation/Stretch & Align Classes
- Wellbeing Coaches
- Steps Challenge
- Workforce Health and Safety
- Financial
- Short Term Loan Program through the GME Office (contact Anna Cardinale)
- Spiritual: Pastoral Care Department
- Columbia (212) 305-5817
- Cornell (212) 746-6971
Family Resources
- Family
- Play Area Association (PAA) www.paanyc.org
- Volunteer social organization run by parents for families of NYPH and affiliated institutions.
- Bright Horizons
- Provides routine and emergency day Care and preschool programs
- Two Locations:
- Columbia Campus: 60 Haven Ave
- Weill Cornell Campus: 435 East 70th St.
- Play Area Association (PAA) www.paanyc.org
Challenges in Training
- Fatigue
- Work load exceeds capacity
- Don’t know what to do in a clinical situation
- Where is my supervisor?
- Who is my supervisor?
- Afraid to ask for help
- Personal illness/life stressors
- Finding time to take care of important business
Fatigue Policy
- We take fatigue seriously and want to know when you are too tired to work
- Our policy
Work load > Capacity Policy
- Our policy
Supervision Policy
- How do you know who your supervisor is?
- How do you reach your supervisor?
- When must you call your supervisor?
- Trigger Policy
- What do you do if you cannot reach your supervisor?
Afraid to ask for help?
- Having trouble with a supervisor?
- Fear of retribution?
- I will get a bad eval
- I will get a bad LOR
- What can you do within the program?
- Who is the go to person in the program
- GME Grievance Policy
Finding time for Personal Business
- Our program is committed to assisting you with find time for taking care of yourself.
- Our policy:
What if you are struggling?
Mental Health Resources
- Housestaff Mental Health Care Resources
- Columbia Campus: Director: Laurel Mayer, MD, Telephone: 646-774- 8067
- Weill Cornell Campus: Director: Scott Goldsmith, MD, Telephone: 212- 439-6309
- Crisis Phone Lines: ER psychiatry attending 24/7
- Columbia 646-426-5190
- Weill Cornell 646-426-5090
- Workforce Health and Safety: confidential employee assistance program that provides mental health and addiction services
- Columbia : Lesley Kondratowic, Nurse Case Manager, 212-305-0861
- Weill Cornell: Mary DeSantis, Nurse Case Manager, 212-746-4370
Taking care of yourself
- Physician take care of yourself!
- Prevention is key
- Don’t wait until there is a crisis
- But if there is a crisis, support is available
- Signs of burn out?
- Is everyone making you crazy?
- There are always options
What if you see someone else struggling?

Sustaining your practice at work and home
- Find joy in what you do at work
- You spend a lot of time here!
- Think of and/or write down three good things that happened at the end of each day
- Find something you are passionate about
- Make time for things you enjoy doing at home
- May need to be spontaneous
- Just do it!...even a little bit of it
